Now a days Mental health struggles like anxiety and depression trigger a cascade of physiological responses that harm the heart. Chronic stress floods the body with cortisol and adrenaline, hormones that increase blood pressure, heart rate, and arterial plaque buildup. Over time, this strain weakens the heart muscle and damages blood vessels. Additionally, inflammation—a common byproduct of prolonged mental distress—accelerates atherosclerosis (hardening of arteries), a leading cause of heart attacks. Studies show individuals with untreated anxiety or depression face a 40% higher risk of cardiovascular disease, with the risks peaking in the 40s due to decades of cumulative stress.
Lifestyle Domino Effect: How Mental Health Impacts Choices
Mental health challenges often lead to unhealthy coping mechanisms that further endanger heart health. Sleep deprivation, poor diet, smoking, or alcohol abuse are common among those battling anxiety or depression. For instance, cortisol-driven cravings for sugary or fatty foods contribute to obesity and diabetes, both linked to heart disease. Similarly, social withdrawal reduces physical activity, weakening cardiovascular resilience. In the 40s, these habits compound with age-related metabolic slowdown, creating a perfect storm for heart attacks. Alarmingly, many dismiss early symptoms like chest tightness or fatigue as “just stress,” delaying critical medical intervention.
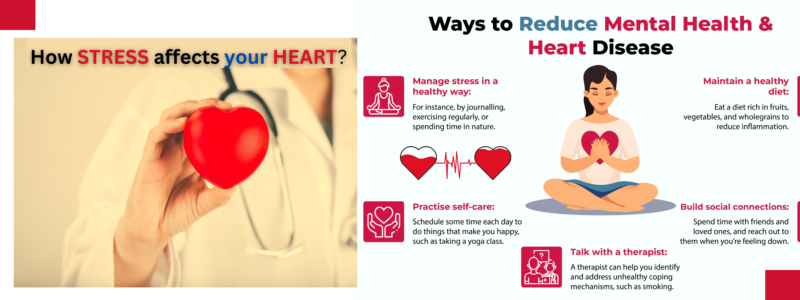
Breaking the Cycle: Proactive Steps for Prevention
Addressing mental health is no longer optional—it’s a cardiovascular necessity. Incorporating mindfulness practices like meditation or yoga can lower cortisol levels and improve heart rate variability. Regular exercise, even light walking, releases endorphins that counteract stress hormones. Therapy or medication for anxiety/depression can disrupt the biological pathways harming the heart. Equally vital is prioritizing sleep and a balanced diet rich in anti-inflammatory foods. Annual heart check-ups after 40 are crucial, especially for those with mental health histories. By treating the mind and body as interconnected systems, we can reverse the tide of preventable heart attacks in this vulnerable age group.
Why Anxiety and Depression Are Skyrocketing in Modern Life
Modern life, with its relentless pace and evolving challenges, has created a perfect storm for mental health crises. Below are key factors driving the surge in anxiety and depression:
Digital Overload and Social Media Pressure
The constant barrage of notifications, comparisons on curated social feeds, and the “always-on” work culture have rewired our brains. Studies link excessive screen time to heightened anxiety, as platforms amplify fear of missing out (FOMO) and unrealistic life benchmarks. The dopamine-driven cycle of likes and shares traps users in a loop of validation-seeking, eroding self-esteem and fueling chronic stress.
Economic Uncertainty and Survival Stress
Skyrocketing living costs, job instability, and gig economy pressures leave many in survival mode. Millennials and Gen Z face unprecedented challenges—student debt, unaffordable housing, and climate anxiety—creating a pervasive sense of helplessness. Financial stress directly correlates with depressive symptoms, as long-term planning feels futile for those struggling to meet basic needs.
Erosion of Community and Loneliness
Urbanization and remote work have fractured traditional support systems. Over 30% of adults report chronic loneliness, a risk factor for depression comparable to smoking. The decline of in-person interactions and community ties leaves individuals without safe spaces to share struggles, amplifying feelings of isolation.
Pandemic Trauma and Its Lingering Shadow
COVID-19 didn’t just disrupt lives—it left deep psychological scars. Grief, health anxiety, and prolonged isolation triggered a 25% global rise in depression and anxiety, per the WHO. Even post-pandemic, uncertainty about health risks and economic recovery lingers, sustaining a low-grade collective dread.
Information Overload and Decision Fatigue
The 24/7 news cycle bombards us with crises—political unrest, climate disasters, and social inequities—leaving minds overwhelmed. Constant exposure to negative content heightens existential anxiety, while endless choices in daily life (career paths, lifestyle trends) paralyze decision-making, breeding self-doubt.
Reduced Stigma Increased Support
While society is more open about mental health, systemic support lags. Workplace burnout is normalized, therapy remains inaccessible for many, and healthcare systems prioritize physical over mental health. Awareness alone can’t bridge the gap between struggles and solutions.
The rise of anxiety and depression isn’t a personal failing—it’s a societal one. Addressing it requires rethinking work cultures, rebuilding communities, and prioritizing mental health infrastructure. Until then, the toll on human well-being will only grow.
Why Stress & Mental Health Harm Hearts in 40s?
The connection between mental health and heart health isn’t just psychological—it’s rooted in biology. Chronic stress, anxiety, and depression trigger physiological responses that directly harm the cardiovascular system. Here’s how the mind-body relationship puts your heart at risk:
Chronic Stress and the Hormonal Onslaught
When the brain perceives stress, it activates the hypothalamic-pituitary-adrenal (HPA) axis, flooding the body with cortisol and adrenaline. These “fight-or-flight” hormones spike blood pressure, accelerate heart rate, and constrict blood vessels to redirect energy. While this response is vital for short-term survival, chronic activation weakens the heart muscle, strains arteries, and promotes plaque buildup. Over time, this can lead to hypertension, arrhythmias, and even heart failure. Research shows that individuals with prolonged stress have double the risk of heart attacks compared to calmer counterparts.
Inflammation: The Silent Accelerator of Heart Disease
Mental health disorders like depression are linked to systemic inflammation. Stress increases cytokines—inflammatory proteins—that damage blood vessel linings (endothelial dysfunction) and accelerate atherosclerosis (hardening of arteries). Inflamed arteries are more prone to plaque rupture, which can trigger clots and blockages. A 2020 study found that adults with depression had 30% higher levels of C-reactive protein, a key inflammation marker, directly correlating with cardiovascular events.
Autonomic Nervous System Imbalance
Anxiety and depression disrupt the autonomic nervous system (ANS), which regulates heart rate, digestion, and breathing. Overactivity of the sympathetic nervous system (responsible for stress responses) paired with underactive parasympathetic activity (responsible for rest) creates an imbalance. This leads to erratic heart rhythms, reduced heart rate variability (a sign of poor resilience), and prolonged recovery after exertion—all predictors of heart disease. Mental health struggles also often lead to unhealthy coping mechanisms, such as smoking, alcohol misuse, poor diet, or physical inactivity—all of which further harm the heart.
Why Its increase day by day?
Modern Lifestyle Pressures:
- People in their 40s today face unprecedented professional, financial, and familial demands. Juggling careers, parenting, and aging parents (the “sandwich generation”) creates chronic stress.
- Work cultures emphasizing long hours, constant connectivity, and job insecurity exacerbate anxiety.
Delayed Mental Health Care:
- Despite growing awareness, stigma often prevents individuals from seeking help early. Untreated stress or depression in younger years compounds by the 40s, worsening heart risks.
Technology and Social Media:
- Constant digital engagement blurs work-life boundaries, reducing downtime. Social media comparisons fuel anxiety and loneliness, even in midlife.
Sedentary Habits and Poor Nutrition:
- Desk jobs, screen time, and reliance on processed foods contribute to obesity, diabetes, and hypertension—key heart disease risk factors amplified by stress.
Economic Instability:
- Rising costs of living, debt, and economic uncertainty in many regions create persistent financial stress, particularly for those in their 40s building careers or supporting families.
Post-Pandemic Fallout:
- The COVID-19 pandemic intensified mental health challenges, isolation, and financial strain, with lingering effects on cardiovascular health.
Prevention and Solutions
- Stress Management: Mindfulness, exercise, and therapy reduce cortisol levels.
- Workplace Reforms: Employers can promote work-life balance and mental health resources.
- Routine Health Screenings: Early detection of hypertension or cholesterol issues mitigates risks.
- Social Support Networks: Building connections counters isolation and improves resilience.
By addressing these root causes, individuals and societies can curb the rising tide of stress-related heart damage in midlife
How Supplements and Mental Health Management Improve Well-Being?
A combination of mental health management strategies and the use of supplements can help enhance both mental and physical well-being.
The Importance of Mental Health Management
Effective mental health management includes practices like mindfulness, therapy, meditation, and regular exercise. These activities reduce stress, improve mood, and enhance cognitive function. Mental health care not only alleviates anxiety and depression but also strengthens emotional resilience, enabling individuals to cope better with life’s challenges.
The Role of Supplements in Well-Being
Nutritional supplements can complement mental health strategies by supporting brain and body function. Key supplements that may improve well-being include:
- Omega-3 Fatty Acids: Known to support brain health and reduce symptoms of anxiety and depression.
- Vitamin D: Helps regulate mood and can counteract the effects of seasonal affective disorder.
- Magnesium: Aids in stress reduction and improves sleep quality.
- Adaptogens: Natural herbs like ashwagandha and rhodiola enhance stress resilience and energy levels.
- Probiotics: Support gut health, which is closely linked to mental health through the gut-brain axis.
The Synergy of Both Approaches
Combining mental health management practices with the right supplements creates a holistic approach to well-being. While mental health strategies address the root causes of stress and anxiety, supplements provide essential nutrients that the body and mind need to function optimally. Together, these strategies promote a healthier lifestyle, greater emotional stability, and improved overall health.
By integrating mental health care and supplementation into daily routines, individuals can achieve a balanced and fulfilling life. Always consult a healthcare professional before starting any new supplement regimen.
Conclusion
Mental health struggles like chronic stress, anxiety, and depression are increasingly linked to heart disease in adults over 40, fueled by modern lifestyle These conditions trigger hormonal imbalances and inflammation, accelerating atherosclerosis and arrhythmias. While lifestyle changes—stress management, exercise, and therapy—remain foundational, certain health supplements may offer supportive benefits. Omega-3s reduce inflammation, magnesium aids blood pressure regulation, and adaptogens like ashwagandha mitigate stress.
FAQs How Mental Health Struggles Fuel Heart Attacks?
Q: How does chronic stress or anxiety increase heart attack risk in your 40s?
A: Prolonged stress triggers the release of cortisol and adrenaline, which raise blood pressure, heart rate, and inflammation. Over time, this damages blood vessels, accelerates plaque buildup (atherosclerosis), and disrupts heart rhythm—key factors in heart attacks.
Q: Can depression directly harm the heart?
A: Yes. Depression is linked to physiological changes like increased inflammation, reduced blood flow, and irregular heart rhythms. It also promotes unhealthy habits Like smoking, poor diet that further strain the heart. Studies show depressed individuals in their 40s have a 30–50% higher risk of heart disease.
Q: Why are people in their 40s more vulnerable now than in the past?
A: Modern lifestyles—constant work pressure, digital overload, financial instability create chronic stress. Additionally, delayed mental health care and stigma mean issues like anxiety or depression often go untreated for years, worsening heart risks by midlife.
Q: How can I protect my heart if I’m struggling with mental health?
A: Prioritize stress management: Mindfulness, yoga, or therapy (CBT) lowers cortisol. Stay physically active 30 minutes of daily exercise improves mood and heart health. Focus on whole foods like fruits, vegetables, whole grains, and lean proteins. Avoid excessive sugar, processed foods and use supplements for a healthy lifestyle or medical treatment but before using this consult a doctor before starting supplements, especially if taking medications.Some important Supplement which is best for today lifestyle are Omega-3 Fish Oil, Magnesium,Vitamin D3,Turmeric/Curcumin etc.
Q: Are heart attacks from mental health struggles preventable?
A: While genetics play a role, lifestyle changes significantly reduce risk. Addressing mental health early, adopting a heart-healthy diet (rich in fruits, vegetables, and omega-3s), quitting smoking, and fostering social connections can mitigate damage. Workplace policies promoting work-life balance and mental health support also play a key role.




Pingback: Anxiety and Heart Risks review by experts | Mindful Nutrition|